Denials in Medical Billing – Offshore Denial Management for USA Providers
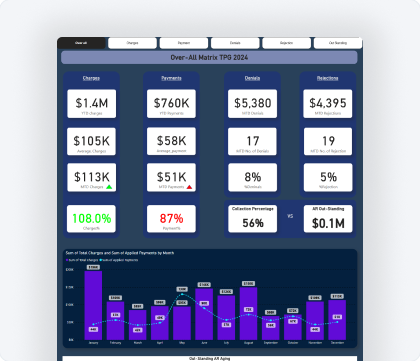
Denials in medical billing are one of the biggest causes of revenue loss for healthcare organizations. Even well-run practices lose thousands of dollars every month due to preventable claim denials, delayed follow-ups, and repeated payer rejections.
InfoHub Consultancy Services is an India-based offshore medical billing company helping USA healthcare providers reduce medical billing denials through structured RCM denial management. We support hospitals, clinics, physicians, doctors, practitioners, and specialty practices by identifying denial root causes, correcting workflows, and aggressively following up on denied claims.
We serve providers across the United States, including California, Texas, Florida, New York, Illinois, Georgia, Arizona, Washington, and New Jersey, while delivering offshore denial management support from India (Coimbatore and Chennai).

 Medical Billing
Medical Billing