Revenue Cycle Management for USA Healthcare Providers (Offshore India Team)
Revenue Cycle Management helps healthcare organizations protect revenue from the first patient interaction to final reimbursement. If your claims are delayed, denials are rising, or AR days are climbing, the root cause is almost always a break somewhere in the revenue cycle management process.
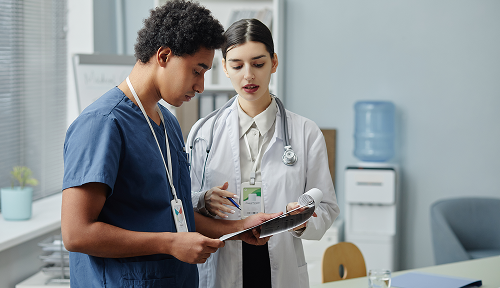
InfoHub Consultancy Services is an India-based offshore medical billing company supporting USA healthcare providers including hospitals, clinics, physician groups, doctors, practitioners, and specialty practices. We help you outsource revenue cycle management from India to the US so you can improve cash flow, control denials, and keep billing operations stable without increasing in-house staffing.
We support providers across the United States, including major markets such as California, Texas, Florida, New York, Illinois, Georgia, Arizona, Washington, and New Jersey, while operating from India (Coimbatore and Chennai).

 Medical Billing
Medical Billing