Behavioral Health Billing
Behavioral health practices operate in one of the most regulated and scrutinized billing environments in healthcare. Frequent CPT updates, evolving CMS policies, payer-specific authorization rules, and rising telehealth utilization make behavioral health billing especially vulnerable to errors and denials.
Behavioral health billing failures rarely stem from lack of care. They happen because of incorrect behavioral health CPT codes, mismatched ICD-10 diagnosis codes, missing modifiers, or breakdowns in revenue cycle coordination. These issues quietly inflate A/R, increase denial rates, and disrupt cash flow.
Info Hub Consultancy Services delivers specialized behavioral health billing services for U.S.-based mental health providers, psychiatry clinics, therapy groups, FQHCs, and community behavioral health centers. Our offshore billing team in India works as an extension of your practice to ensure accuracy, compliance, and financial stability across commercial insurance, Medicaid, and Medicare.

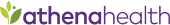
 Medical Billing
Medical Billing 



























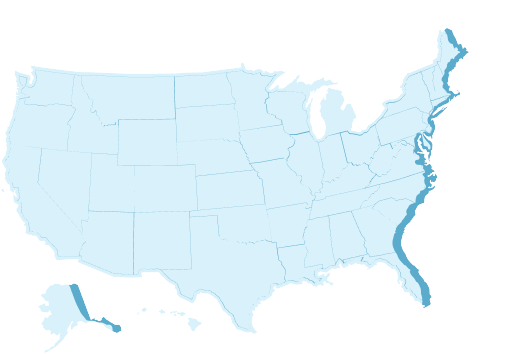
 Trusted by 140+ Providers in All 50 States
Trusted by 140+ Providers in All 50 States