Is your medical billing and coding structure truly protecting your revenue cycle, or has it gradually reduced your operational control? The issue often extends beyond day-to-day billing performance when reimbursements slow down, denial rates fluctuate, or reports lack clarity. In many situations, the root cause lies in how billing resources are organized and managed.
Healthcare practices now operate in a reimbursement environment that demands coding precision, regulatory awareness, and timely follow-up. Payer policies continue to evolve, documentation requirements are closely scrutinized, and even small coordination gaps can affect financial outcomes. As a result, the decision between a Dedicated Full-Time Equivalent model and a Shared Billing Team becomes more than a staffing choice. It becomes a strategic decision that shapes oversight, accountability, and long-term revenue stability.
This blog will examine the differences between Dedicated FTE and Shared Billing Teams and outline the key considerations to guide the hospitals.
Overview of the Billing Models
Under the Dedicated FTE model, specific billing and coding professionals work exclusively for one practice and function as an extension of its internal team. This structure allows deeper familiarity with the practice’s specialty, EMR system, payer mix, and documentation patterns.
In contrast, the Shared Billing Team model distributes billing responsibilities across a pooled group of professionals who handle multiple client accounts simultaneously. Though this shared approach offers scalability and variable cost structures, it often relies on standardized workflows designed to serve diverse provider types rather than one practice’s specific operational needs.
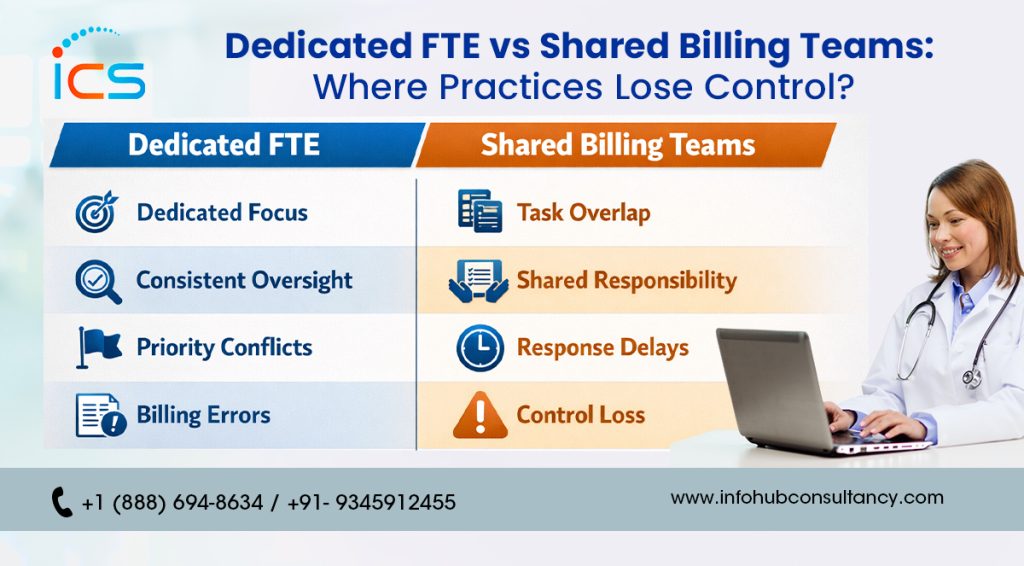
Where Practices Lose Control: Shared Billing Teams
Although this model may appear financially attractive in the beginning, pooled billing resources generally follow broad protocols that do not always reflect specialty-specific coding nuances.
-
Limited Claim Prioritization in Billing Queues
As shared billing professionals manage accounts for multiple healthcare providers simultaneously, claims often enter generalized work queues. Consequently, complex or high-revenue specialty claims may not receive immediate, focused attention. Even when turnaround benchmarks are technically met, the absence of exclusive handling can delay appeals, coding corrections, and payer-specific follow-ups.
-
Reduced Transparency in Coding and Claim Status
When staffing rotates across several accounts, identifying who coded a particular claim or managed a denial becomes more difficult. As a result, obtaining detailed explanations may require additional coordination, which can slow internal decision-making. Without consistent ownership, tracking payer behavior, modifier usage patterns, or recurring rejection causes becomes less precise and more reactive.
-
Inconsistent Coding Interpretation
Within a shared billing pool, different coders may interpret documentation guidelines in slightly different ways. Although these variations may appear minor, small differences in CPT, ICD-10, or modifier application can influence reimbursement outcomes. Therefore, such inconsistencies may increase denial rates and generate unnecessary rework within the revenue cycle.
-
Standardized Processes Over Specialty Customization
Shared billing vendors typically rely on uniform workflows designed to accommodate a wide range of provider types. However, specialty practices often require payer-specific coding adjustments and customized follow-up strategies. When workflows remain generalized, adapting billing processes to match clinical complexity and documentation preferences becomes more challenging.
Where Practices Retain Control: Dedicated FTE Model
In this structure, the billing team operates as a direct extension of the provider’s internal staff, which strengthens operational alignment.
-
Direct Oversight of Coding Quality and Compliance
Under a dedicated model, the practice team can clearly define expectations for documentation review, coding standards, and denial workflows. At the same time, daily supervision ensures that billing activities align with regulatory guidelines and payer policies. When coding updates or compliance changes occur, adjustments can be implemented quickly and consistently.
-
Deeper Familiarity With EMR and Specialty Codes
As dedicated coders work continuously with the same practice, they develop a strong understanding of EMR templates, provider documentation patterns, and commonly billed procedures. This growing familiarity improves coding precision and strengthens first-pass claim acceptance rates. Additionally, the need for repetitive clarifications gradually decreases.
-
Focused Denial Management and Appeals
As the billing professional concentrates solely on one account, denial trends are monitored more closely and analyzed more thoroughly. Instead of addressing issues sporadically, corrective strategies can be introduced proactively. As a result, resolution timelines shorten and accounts receivable performance becomes easier to manage.
-
Stable Performance and Revenue Consistency
Working with the same billing and coding team eliminates repeated onboarding cycles and workflow disruptions. Over time, institutional knowledge builds steadily and supports predictable operational performance. This continuity contributes to consistent cash flow and reduces interruptions caused by frequent staffing changes.
The Control Trade-Off
When comparing dedicated FTE and shared billing teams, the central consideration revolves around control versus flexibility. A dedicated FTE model provides higher operational oversight as the practice directs daily billing activities, monitors coding quality closely, and implements workflow adjustments as needed. In fact, this level of involvement strengthens accountability and supports long-term revenue stability. However, it typically requires a fixed monthly financial commitment regardless of fluctuations in claim volume.
On the other hand, a shared billing team offers adaptability, especially for practices experiencing variable patient volumes or seasonal demand changes. Costs often align with claim volume or collections, which can ease short-term financial pressure. Nevertheless, this flexibility may limit direct supervision, reduce workflow customization, and dilute ownership of performance outcomes. Therefore, the decision depends on whether a practice prioritizes structured oversight and consistency or prefers scalable resources with variable expense commitments.
Key Considerations for Your Medical Practice
A structured comparison helps ensure that the chosen billing model aligns with both operational needs and long-term financial objectives.
-
Practice Volume and Clinical Complexity
Flexibility and reduced overhead may be primary considerations for lower-volume primary care clinics. In contrast, multi-specialty or high-volume practices often require structured coding oversight and detailed monitoring. The level of documentation complexity and payer variation should guide the choice of billing structure.
-
Need for Detailed Revenue Reporting
Practices that depend on granular denial analytics, coding audits, and real-time financial visibility typically benefit from consistent accountability. Dedicated staff provide clearer insight into claim performance and workflow metrics. However, practices with simpler reporting requirements may find shared service arrangements sufficient.
-
Future Expansion and Service Diversification
Growth initiatives often demand a billing framework capable of adapting to new services, payer contracts, or compliance updates. Dedicated resources gradually accumulate practice-specific expertise that supports long-term scaling efforts. Though shared teams offer adaptability, they may provide less continuity for sustained strategic development.
-
Budget Predictability and Cost Structure
A dedicated FTE involves a fixed monthly investment, which supports stable budgeting and expense forecasting. On the other hand, shared billing models commonly operate on per-claim or percentage-based pricing, resulting in variable costs. The preferred option depends on whether predictable expenses or scalable pricing better align with the practice’s financial strategy.
Conclusion
Selecting the right medical billing and coding structure ultimately shapes how effectively a practice safeguards its revenue and maintains operational clarity. Though both engagement models serve legitimate purposes, the decision should align with the practice’s long-term financial vision, specialty requirements, and desired level of administrative involvement. A thoughtful evaluation ensures that billing operations support stability rather than create hidden inefficiencies.
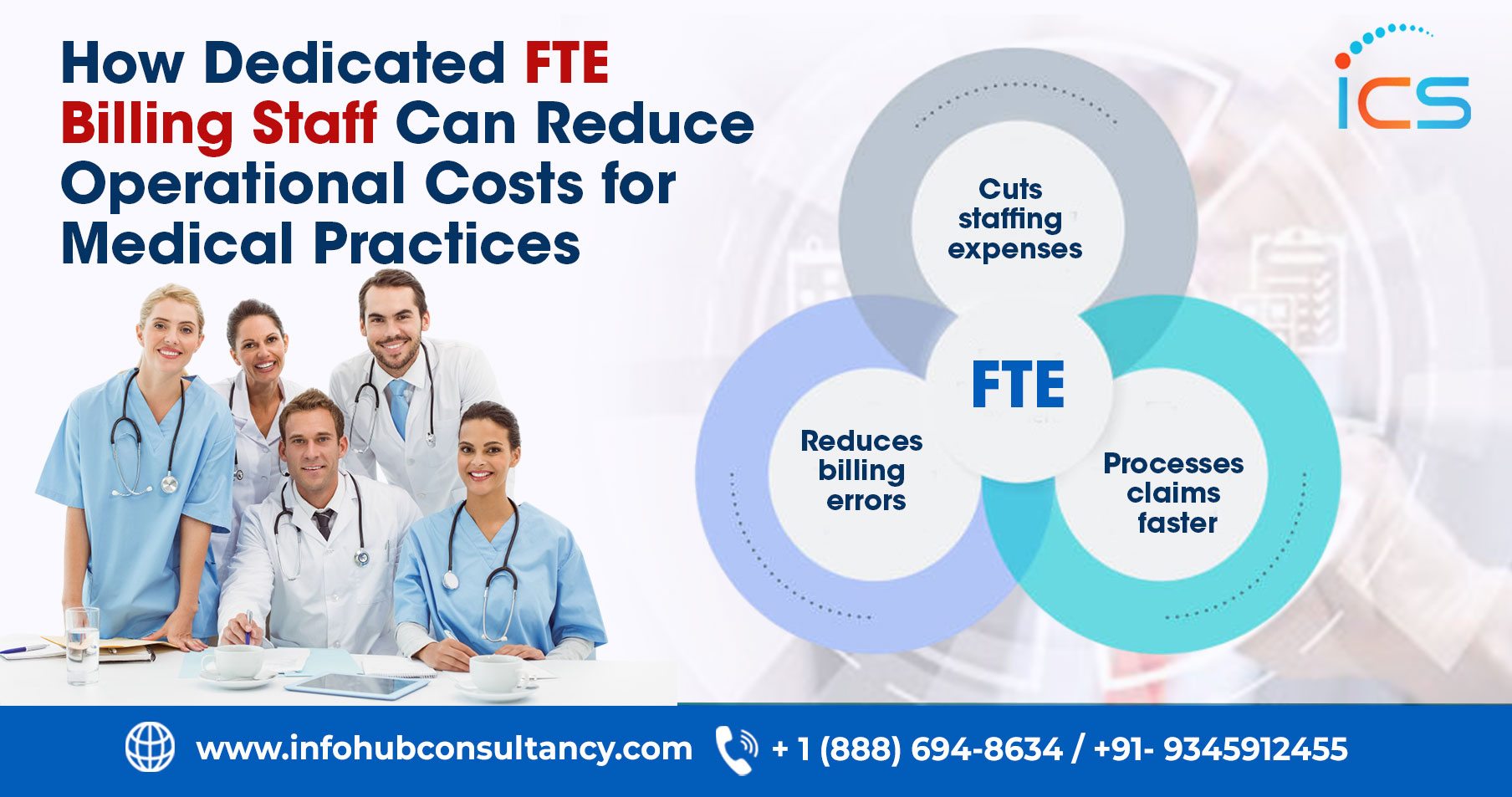
In fact, a dedicated approach often delivers stronger strategic value for practices seeking structured oversight, deeper workflow alignment, and sustained revenue performance. InfoHub Consultancy Services delivers dedicated FTE staffing to help U.S. practices streamline operations, reduce denials, and improve reimbursements. Therefore, ICS enables healthcare organizations to strengthen financial performance by combining focused expertise with consistent accountability.
FAQs
How does billing team structure affect compliance audits?
A clearly assigned billing structure improves documentation traceability and strengthens audit preparedness.
Which model supports better data security controls?
Dedicated teams often allow tighter access management aligned with internal security protocols.
How does team structure influence turnaround time for AR cleanup?
Focused billing resources typically address aging accounts more systematically.

 Medical Billing
Medical Billing  7 mins read
7 mins read