Telehealth has become an essential part of modern healthcare, but are practices truly prepared to navigate its billing challenges?
What happens when claims are submitted incorrectly or documentation is incomplete?
Even small mistakes can disrupt revenue and create compliance risks. With so many changes, how can providers ensure accuracy and efficiency?
This blog will discuss the key guidelines for telehealth billing in 2026.
Telehealth Billing: Key Guidelines for 2026
Telehealth billing in 2026 requires practices to follow structured rules around coverage, coding, documentation, patient location, and compliance. Temporary flexibilities from the public health emergency are largely phased out, making adherence to Medicare requirements essential. Providers must verify service eligibility, follow proper coding, and maintain accurate documentation to prevent claim denials, audits, or payment recoupments, ensuring compliant, financially secure telehealth operations.
Medicare Telehealth Coverage Guidelines
In 2026, Medicare covers only a defined list of telehealth services, and many temporary services are no longer reimbursable. Behavioral health services retain broader coverage, whereas other services often require in-person care. Practices must confirm service eligibility before scheduling or billing, using updated Medicare resources. This verification helps prevent claim denials and payment delays and ensures consistent compliance across all virtual services.
Geographic and Originating Site Guidelines
Medicare reinstates geographic and originating site restrictions for most services in 2026. Patients must generally be in eligible rural areas or approved medical facilities. Home-based visits are limited except for specific behavioral health care. Practices must document patient location at each encounter, as accurate location reporting is required for claims, supports compliance, and reduces the risk of denied or rejected telehealth submissions.
Behavioral Health Telehealth Billing Rules
Behavioral health services continue to receive permanent telehealth coverage, including video and audio-only visits when appropriate. Providers must ensure at least one in-person visit within a defined timeframe for ongoing care, unless an exception applies. Documentation of compliance is required in the medical record. Proper tracking and recording help maintain service eligibility, reduce claim denials, and support safe and compliant virtual behavioral health delivery.
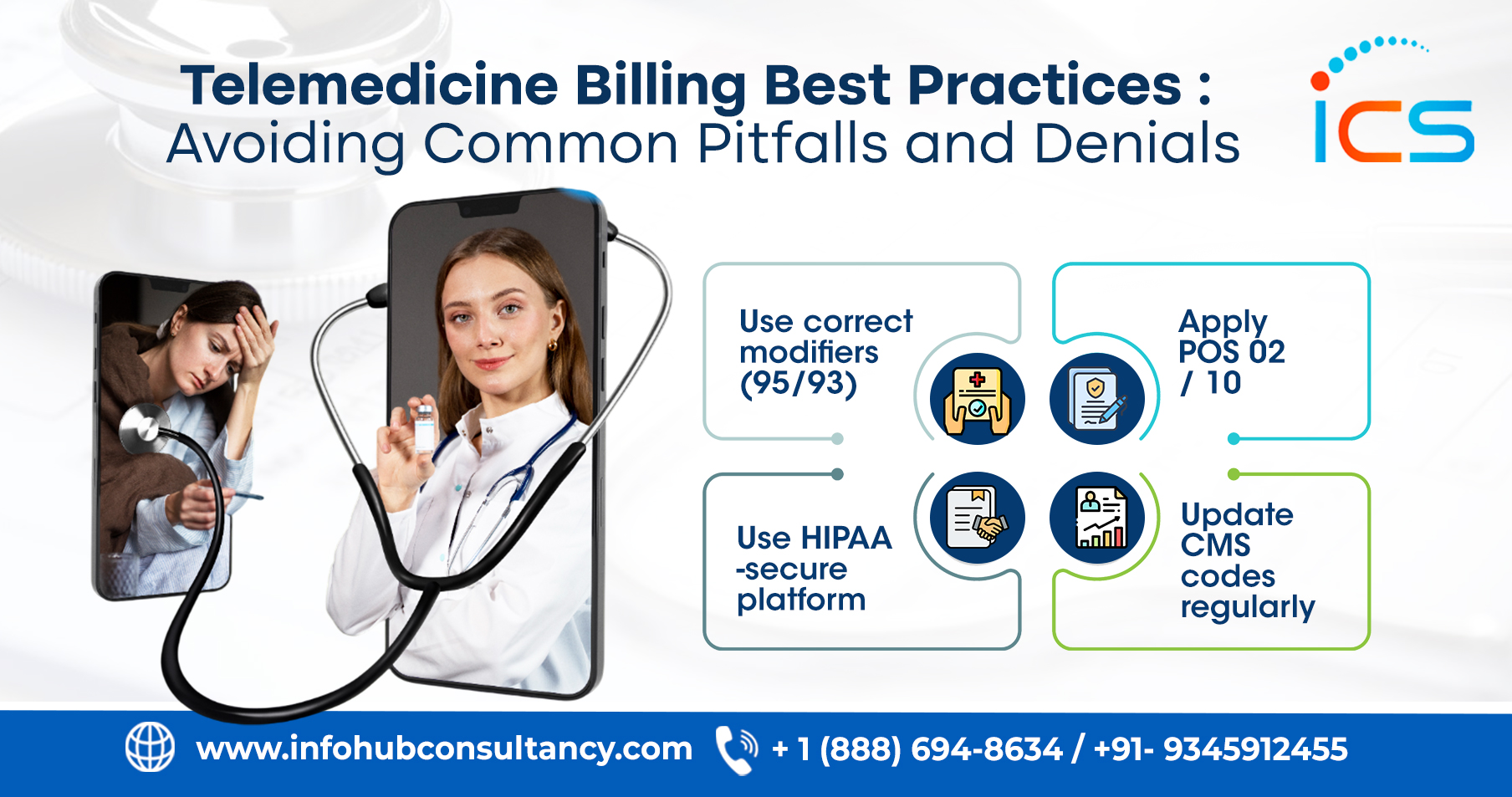
Place of Service and Modifier Requirements
In 2026, accurate POS reporting is critical for telehealth claims. POS 02 is used when care occurs outside the patient’s home, while POS 10 is required at the patient’s residence. Incorrect POS or missing modifiers can lead to reduced reimbursement or claim rejection. Billing teams must closely follow payer-specific guidance to ensure proper payments, minimize errors, and maintain audit readiness.
CPT and E/M Coding Guidelines
Telehealth visits must be billed using standard CPT and E/M codes based on provider time or medical decision-making. Documentation must support code selection and meet the same standards as in-person visits. Incomplete records increase audit risk and may cause downcoding or denials. Accurate, consistent coding ensures compliant reimbursement and aligns clinical documentation with telehealth billing requirements for all encounters.
Audio-Only Telehealth Billing Guidelines
Audio-only billing is limited to behavioral health services in 2026. Providers must document why the video was unavailable or inappropriate and confirm clinical necessity. In fact, other specialties are generally not reimbursed for audio-only visits. Verification of patient eligibility, payer requirements, and supporting documentation is essential to prevent claim denial. Proper records help ensure compliant reimbursement and reduce the risk of payment reversal.
Remote Patient Monitoring and Digital Health Billing
Remote patient monitoring remains reimbursable under defined CPT codes. Billing requires documented patient consent, eligible devices, active data collection, and minimum time thresholds. Providers must track time spent on clinical decision-making and patient engagement. Incomplete documentation can lead to denials. Accurate reporting ensures compliance with Medicare standards, supports program sustainability, and enables safe remote monitoring of chronic conditions or patient health trends.
Technology and Documentation Requirements
Practices must use EHRs and management systems to document visit modality, patient location, provider time, and consent. Automated billing edits and prompts can reduce errors. Clear records showing services were delivered via telehealth are necessary for audits. Staff training ensures consistent documentation practices. Investing in technology readiness and thorough documentation helps reduce denials, expedite reimbursement, and support ongoing regulatory compliance.
Compliance and Audit Readiness Guidelines
Medicare audits telehealth claims more closely in 2026. Practices must maintain accurate coding, documentation, and billing records. Regular internal audits identify gaps early and support corrective measures. Monitoring payer updates ensures ongoing adherence to policy changes. A proactive compliance strategy protects practices from recoupments, penalties, and revenue loss, supporting stable telehealth operations while enhancing long-term confidence in billing practices.
Patient Consent Requirement
All telehealth services require documented patient consent, which can be verbal if recorded in the medical record. In fact, the prior consent confirms that patients understand virtual care delivery and agree to participate. Without proper consent, claims risk denial. Providers should verify, record, and retain consent for each encounter. Consistent documentation safeguards compliance, reduces payment risk, and provides a strong defense during audits or reviews.
Provider Eligibility and Credentialing
Only eligible providers, including physicians, nurse practitioners, physician assistants, and behavioral health providers, can bill Medicare for telehealth. Providers must be appropriately credentialed and enrolled, ensuring compliance with federal rules. Billing by ineligible staff can lead to denials or audits. Practices should verify provider eligibility before submitting claims to maintain compliant billing, accurate reimbursement, and avoid potential financial penalties.
Frequency and Visit Limitations
Certain telehealth services have a maximum number of allowed visits within specific timeframes. Billing beyond these limits can trigger denials or audits. Practices must monitor how often patients receive particular services and ensure claims reflect allowable frequencies. Tracking visit patterns helps avoid overbilling, supports Medicare compliance, and ensures proper reimbursement. Adhering to these rules safeguards revenue while maintaining quality telehealth care delivery.
Time Documentation Standards
It is important to remember that only direct patient care time is billable for time-based telehealth billing, excluding administrative tasks. Providers must accurately document total service time. Precise time records ensure proper CPT/E/M code selection and prevent underpayment or claim rejection. Practices should integrate time-tracking protocols and verify the completeness of documentation. Therefore, consistent time documentation supports compliant billing, protects against reimbursement issues, and strengthens audit readiness.
Split/Shared Telehealth Services
Medicare allows split or shared E/M visits in telehealth when multiple providers contribute. Documentation must clearly reflect each provider’s involvement and identify the billing provider. Accurate records prevent denials and ensure correct reimbursement. Practices using team-based care must establish workflows to track contributions, maintain documentation integrity, and support compliant billing practices across all shared telehealth encounters.
One Stop Solution: Outsourcing Telehealth Billing and Coding Services in India
Offshore telehealth billing and coding services in India to InfoHub Consultancy Services provide practices with a reliable, efficient way to comply with the detailed 2026 guidelines. ICS ensures every claim is accurately coded, adequately documented, and fully compliant with Medicare and payer-specific requirements, minimizing denials and audit risks. Their team tracks patient consent, visit limits, and time-based billing while seamlessly managing split/shared services. Also, ICS keeps practices aligned with evolving telehealth rules by staying up to date on regulatory changes. This allows providers to improve revenue cycle efficiency and maintain financial stability, making outsourcing a strategic choice for telehealth success.
FAQs
Do all insurers accept telehealth claims electronically?
Most insurers accept electronic claims, but checking payer-specific requirements is essential.
How quickly are telehealth claims reimbursed?
Reimbursement timelines vary by payer, but proper coding and documentation can speed approval.
Are there reporting requirements for telehealth billing?
Yes, practices should track volumes, denials, and reimbursements for audits and performance.

 Medical Billing
Medical Billing  7 mins read
7 mins read