Ever looked at a medical bill and wondered how that doctor’s visit for a sore throat transformed into a string of numbers and a specific dollar amount? You’re not alone. The back-end of healthcare finance feels like a foreign language to most. But here’s the thing: that complex translation is the lifeblood of every clinic and hospital. It’s handled by two critical yet distinct fields: medical coding and medical billing.
People often use the terms interchangeably, but that’s like saying an author and a publisher do the same job. One creates the core content; the other packages and brings it to market. In healthcare, coders and billers are specialized partners in a critical relay race. Mixing them up can lead to real confusion about career paths, practice management, and where revenue bottlenecks lie. So, let’s clear the air. What exactly sets them apart, and how do they work together to keep healthcare providers paid and patients billed correctly?
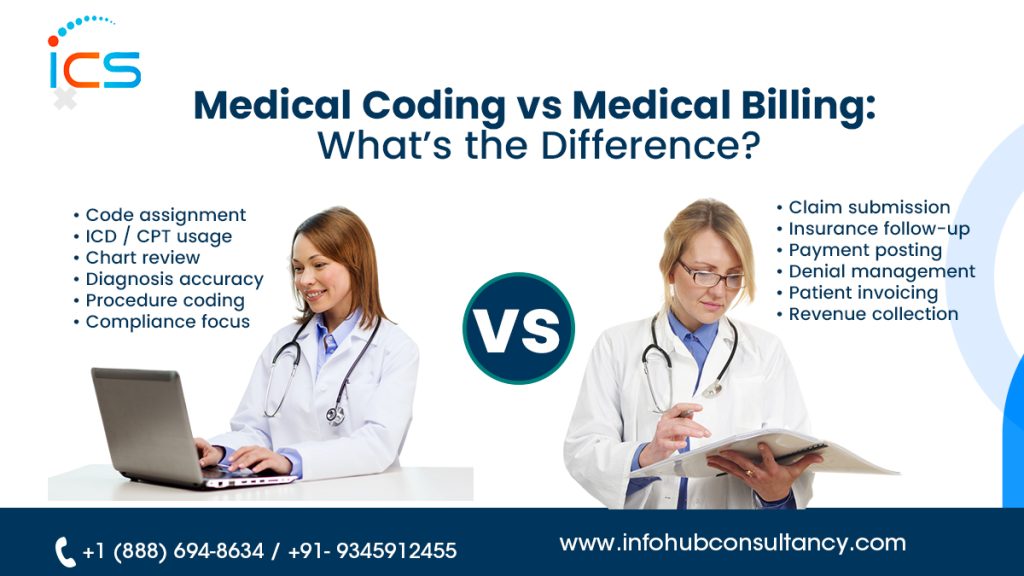
The Core of the Confusion: Why They Seem So Similar
First, it’s easy to see why the lines blur. Medical coding and billing are closely intertwined processes that operate in parallel within the revenue cycle management (RCM) pipeline. They share the same ultimate goal: to ensure healthcare providers are accurately reimbursed for their services. Both require a sharp eye for detail, a solid understanding of medical terminology, and a commitment to compliance.
They work from the same source document: the patient’s medical record. In many smaller practices, one person might wear both hats—handling translation (coding) and submission (billing). But that’s where the similarity ends. In reality, they are separate disciplines with unique skill sets, responsibilities, and challenges. Think of it this way: coding is about what happened; billing is about getting paid for what happened.
Medical Coding: The Art of Translation
If medical billing is the business side, medical coding is the linguistic and analytical foundation. This is where clinical information gets transformed into a universal, standardized code.
Imagine a doctor writes in a chart: “Patient presented with acute dyspnea and wheezing, diagnosed with acute bronchospasm, administered albuterol nebulizer treatment.” To an insurance company or a national database, that narrative is too vague. They need a precise, alphanumeric shorthand. That’s the coder’s job.
What does a medical coder actually do?
- Review Clinical Documentation: Coders meticulously read physician notes, operative reports, lab results, and radiology findings. They need to understand the patient’s account of the visit.
- Assign Codes: Using standardized code sets, they translate every diagnosis, procedure, service, and piece of equipment into specific codes.
- ICD-10-CM: These codes describe the diagnosis (e.g., J45.909 for Unspecified asthma, uncomplicated).
- CPT/HCPCS: These codes describe the procedures, services, and supplies (e.g., *94640* for that albuterol nebulizer treatment).
- Ensure Accuracy and Specificity: This is the crux of the job. Was it simple asthma or an acute exacerbation? Was the procedure moderate or high complexity? Choosing the wrong code isn’t just an administrative error—it can lead to claim denials, compliance issues, or even accusations of fraud.
The Coder’s Mindset: Precision is king. Coders are detectives, looking for details in the documentation to justify the most accurate code. They live in the world of guidelines, updates (these code sets change annually!), and clinical nuance. Their primary question is: “Does this code exactly represent what the provider documented?”
Medical Billing: The Engine of the Revenue Cycle
Now, take those meticulously assigned codes. They’re raw data. Medical billing is the process of taking that coded data and turning it into a financial claim, then shepherding that claim through the payment pipeline.
The biller takes the coder’s output and uses it to create the “bill,” though in healthcare, it’s called a claim. They’re the advocates and negotiators who deal directly with insurance companies and patients.
What does a medical biller actually do?
- Claim Creation and Scrubbing: Using the codes provided, billers fill out the standardized claim form (usually the CMS-1500 or UB-04). They then “scrub” the claim, checking for errors like mismatched codes, missing patient information, or incorrect policy numbers before it’s sent.
- Submission and Follow-Up: They electronically submit claims to insurers, then track them relentlessly. Did it get received? Adjudicated? Paid? Denied?
- Managing Payments and Denials: When an Explanation of Benefits (EOB) comes back, the biller reconciles it. Was the payment correct? If a claim is denied, they investigate why (was it a coding error, a policy limit, a clerical mistake?) and take action—whether that’s correcting and resubmitting the claim or appealing the decision.
- Patient Billing and Communication: After insurance pays its share, the biller generates statements for patient balances. They also field questions from confused patients about their bills, requiring a blend of financial and customer service skills.
The Biller’s Mindset: Persistence and communication are key. Billers are like project managers for money. They follow up, negotiate, and problem-solve, and they need a thick skin to handle payer policies and frustrated patients. Their primary question is: “How do I get this claim paid correctly and completely?”
Side-by-Side: The Key Differences Broken Down
- Claim Creation and Scrubbing: Using the codes provided, billers fill out the standardized claim form (usually the CMS-1500 or UB-04). They then “scrub” the claim, checking for errors like mismatched codes, missing patient information, or incorrect policy numbers before it’s sent.
- Submission and Follow-Up: They electronically submit claims to insurers, then track them relentlessly. Did it get received? Adjudicated? Paid? Denied?
- Managing Payments and Denials: When an Explanation of Benefits (EOB) comes back, the biller reconciles it. Was the payment correct? If a claim is denied, they investigate why (was it a coding error, a policy limit, a clerical mistake?) and take action—whether that’s correcting and resubmitting the claim or appealing the decision.
- Patient Billing and Communication: After insurance pays its share, the biller generates statements for patient balances. They also field questions from confused patients about their bills, requiring a blend of financial and customer service skills.
The Biller’s Mindset: Persistence and communication are key. Billers are like project managers for money. They follow up, negotiate, and problem-solve, and they need a thick skin to handle payer policies and frustrated patients. Their primary question is: “How do I get this claim paid correctly and completely?”
Side-by-Side: The Key Differences Broken Down
Let’s make this crystal clear. Here’s a direct comparison.
| Feature | Medical Coding | Medical Billing |
| Primary Focus | Translating clinical care into standardized codes. | Submitting claims and securing payment. |
| Core Skill | Analytical, detail-oriented, strong grasp of anatomy, terminology, and coding guidelines. | Administrative, communicative, and knowledge of insurance guidelines and payer processes. |
| Key Tools | Code books (ICD-10-CM, CPT, HCPCS), encoder software, and medical records. | Practice Management Software (PMS), billing software, clearinghouses, EOBs. |
| End Product | An accurately coded patient encounter. | A clean claim, followed by payment collection. |
| Patient Interaction | Virtually none. Works with documents. | Frequent, especially regarding billing questions and payment plans. |
| Biggest Challenge | Interpreting ambiguous documentation; keeping up with annual code changes. | Managing claim denials and appeals; navigating complex payer rules. |
The Handoff: How Coding and Billing Work Together in the Revenue Cycle
This isn’t a theoretical separation. It’s a daily, operational workflow. Here’s how the baton gets passed:
- Patient Visit: The provider sees the patient and documents the visit in the medical record.
- The Coder’s Stage: The medical coder reviews the record, assigns the correct diagnosis and procedure codes, and enters them into the practice management system.
- The Biller’s Stage: The medical biller takes the coded encounter, verifies patient insurance details, creates the claim, scrubs it for errors, and submits it to the insurance payer.
- The Follow-Through: The biller tracks the claim, posts payments when they arrive, handles any denials (which may require going back to the coder for clarification), and bills the patient for the remaining balance.
See the dependency? If the coder drops the ball—uses an outdated or incorrect code—the biller’s claim is dead on arrival. Conversely, if the biller submits a perfect code with the wrong patient ID, the coder’s perfect work is wasted. They are two halves of a whole system.
Why Understanding the Difference Matters (For More Than Just Semantics)
This isn’t just academic. Knowing the distinction has real-world implications.
- For Healthcare Practices: Understanding the separate functions helps in hiring, managing workflow, and identifying bottlenecks. Is your revenue low due to coding errors or billing follow-up failures? The solution is different for each.
- For Aspiring Professionals: If you’re considering a career in healthcare administration, this is crucial. Do you love language, detail, and working independently with data? Coding might be your path. Are you a natural communicator, problem-solver, and persistent advocate? Billing could be a better fit.
- For Patients: Knowing there are dedicated professionals ensuring accuracy can be reassuring. It also helps you understand why a billing issue might occur—it could stem from a coding translation error or an insurance payer’s specific rule.
Two Fields, One Goal: A Conclusion on Collaboration
So, medical coding vs. medical billing? It’s not a versus at all. It’s a partnership. One cannot succeed without the other. The coder builds the foundation with precision codes; the biller constructs the financial house upon it. In a world of ever-changing regulations and complex insurance landscapes, both roles are more vital than ever.
For a healthcare practice to thrive, it needs both the analytical depth of skilled coders and the tenacious follow-through of expert billers. Investing in both—whether through training, technology, or specialized staffing—isn’t an overhead cost; it’s an investment in a healthy, sustainable revenue cycle.
If you’re running a practice and feeling the pinch of delayed reimbursements or high denial rates, take a closer look at your relay team. Are your coders and billers in sync? Do they have the tools and clarity they need? Sometimes, the first step to improving your practice’s financial health is simply understanding the distinct yet interconnected roles that keep it running. And if you need help optimizing that partnership, that’s where expert guidance can make all the difference.
Frequently Asked Questions (FAQs)
What is the main difference between medical coding and medical billing?
Medical coding focuses on translating clinical documentation into standardized codes like ICD-10, CPT, and HCPCS. Medical billing uses those codes to create claims, submit them to insurance companies, follow up on payments, and bill patients for any remaining balance.
Which is more important: medical coding or medical billing?
Neither is more important—they’re equally critical. Even perfect coding won’t get paid if the billing follow-up is weak. And strong billing can’t fix incorrect or incomplete coding. Both must work together to maintain a healthy revenue cycle.
Do coding errors always lead to claim denials?
Not always, but they significantly increase the risk. Incorrect or nonspecific codes can result in denials, underpayments, audits, or compliance issues. Accurate coding is one of the best ways to reduce avoidable denials.
How does medical coding affect revenue cycle management (RCM)?
Medical coding directly impacts claim acceptance, reimbursement accuracy, and compliance. Poor coding can lead to denials and delays, while accurate coding enables faster payments and cleaner claims throughout the RCM process.
What happens when a claim is denied due to a coding or billing issue?
The medical biller reviews the denial reason, corrects the issue if possible, and resubmits or appeals the claim. In many cases, this may require clarification or correction from the coding team, which is why collaboration is essential.

 Medical Billing
Medical Billing  9 mins read
9 mins read