What does it mean when nearly one in every seven medical claims is denied, and each denied claim costs providers over $25 to rework?
What happens when days in accounts receivable continue to rise, while operating margins across healthcare remain under pressure?
In 2026, these outcomes are becoming more common, not exceptional. In fact, they directly affect cash flow, staffing stability, and financial sustainability when billing challenges are ignored. That is why it is critical to understand what has changed for U.S. healthcare providers in 2026.
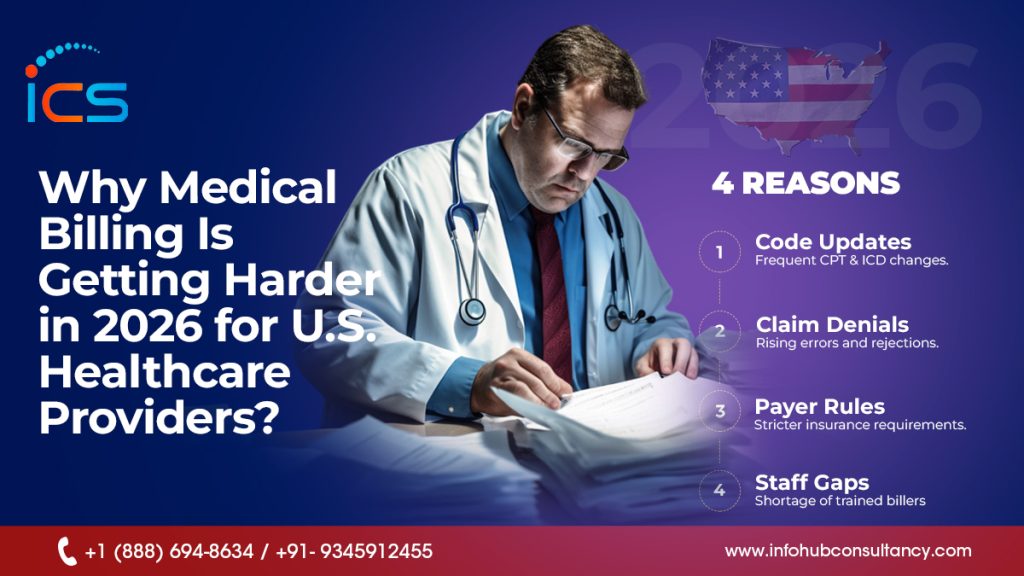
This blog explains why medical billing is becoming more difficult in 2026 and why providers must be prepared
Stricter Compliance Rules
Healthcare regulations in 2026 require much higher levels of compliance across billing operations. In fact, federal standards and payer-specific policies continue to tighten, requiring accurate documentation, secure data handling, and precise claim submission. As a result, even minor compliance errors can lead to penalties or rejected claims. Billing teams must constantly track regulatory changes while managing daily workloads. This growing compliance burden increases administrative effort and makes medical billing more demanding for providers.
Faster Prior Authorization
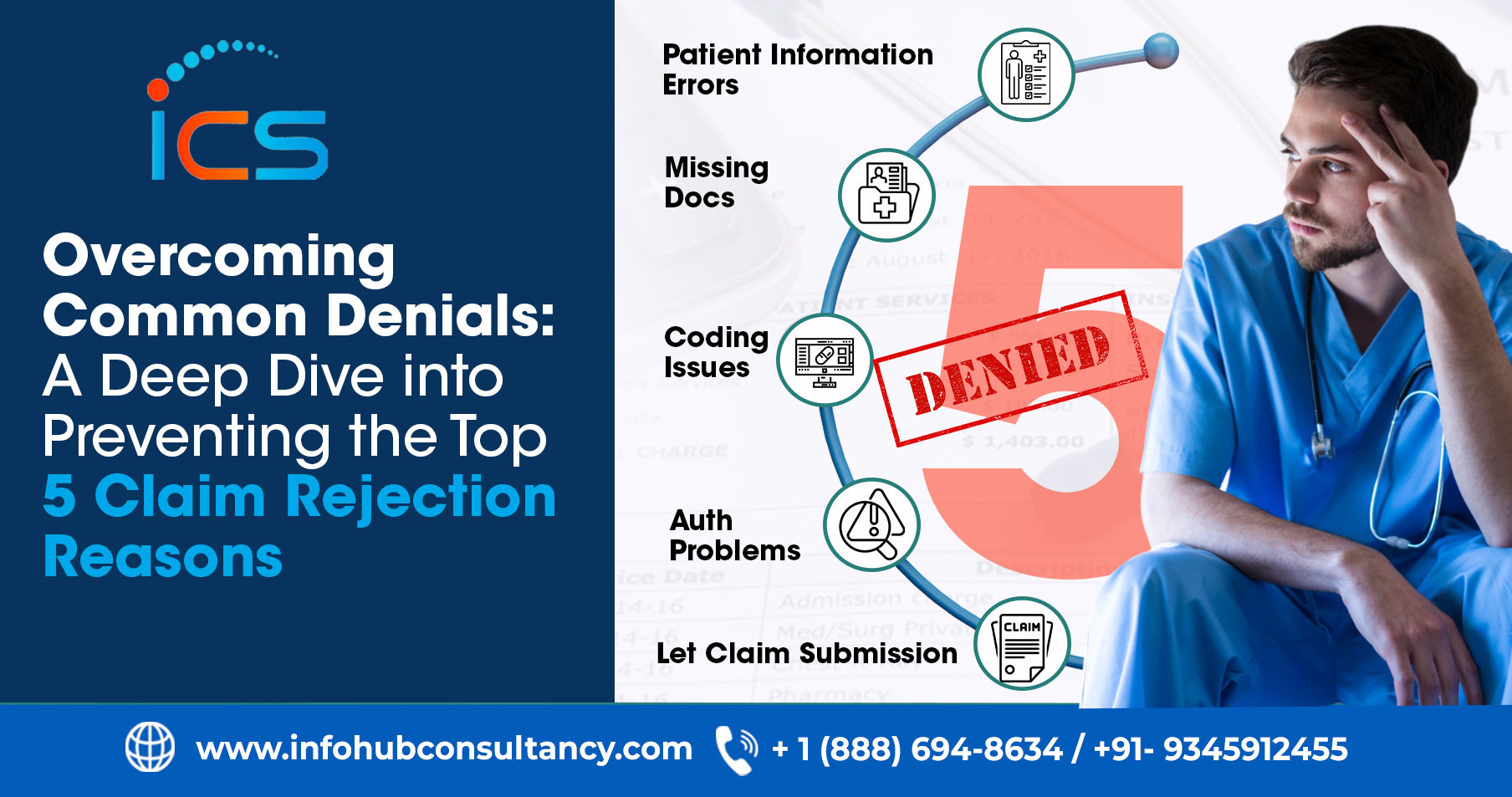
Prior authorization requirements in 2026 place increased pressure on billing teams. Payers now expect electronic submissions and faster approval timelines for many services. When authorization details are incomplete or delayed, claims are often denied before payment begins. As a result, practices struggle to keep up with the volume and speed required. This added responsibility slows billing workflows, increases administrative tasks, and makes timely reimbursement more challenging.
Frequent Coding Changes
Medical billing accuracy is harder to maintain in 2026 due to frequent CPT and ICD-10 updates. New codes are introduced, whereas others are revised or removed, requiring constant training and system updates. Thereby, claims are rejected or underpaid when codes do not match the services provided. Therefore, billing teams must ensure precise coding for every encounter. As a result, keeping up with these changes increases complexity and raises the risk of costly billing errors.
Higher Documentation Standards
Documentation expectations have increased significantly in 2026. Payers now require detailed clinical notes that clearly support medical necessity and align with billed codes. When documentation is incomplete or unclear, claims are more likely to be denied. Billing teams often need clarification from providers, which delays submission. As a result, billing success depends more heavily on accurate clinical documentation and strong coordination between clinical and billing staff.
Rising Claim Denials
Claim denials are more common in 2026 due to stricter payer reviews and technical requirements. Many denials result from authorization issues, coding mismatches, or missing information rather than clinical errors. In fact, each denied claim requires additional work, including corrections and appeals. Consequently, billing teams spend more time resolving issues instead of processing payments. This ongoing rise in denials slows cash flow and strains operations.
AI-Based Claim Reviews
Payers increasingly rely on artificial intelligence to review claims in 2026. These systems quickly detect errors, inconsistencies, and missing details. In particular, high-cost claims are subject to additional scrutiny and are often automatically denied if requirements are not met. As a result, billing teams must ensure claims are entirely accurate before submission. This automation increases pressure on billing operations and leaves little room for manual adjustments.
Value-Based Payment Models
Billing has become more complex as value-based reimbursement models expand in 2026. Payments are now tied to patient outcomes and quality performance rather than solely to service volume. Therefore, billing teams must capture additional data and ensure accurate reporting. This shift requires closer coordination between clinical and administrative teams. The added reporting responsibilities increase workload and make billing processes more complicated.
Staffing Shortages
Staffing shortages continue to impact billing departments in 2026. With fewer experienced professionals available, the remaining staff must manage larger workloads. As pressure increases, the risk of errors and delays also rises. Training new employees becomes more difficult due to constant regulatory and coding changes. As a result, limited staffing makes it harder to maintain billing accuracy and operational efficiency.
Patient Payment Collection
Patient financial responsibility has increased in 2026 due to higher deductibles and out-of-pocket costs. Providers must now collect a larger share of revenue directly from patients. As a result, billing teams spend more time explaining charges, managing payment plans, and following up on balances. In fact, delayed payments affect cash flow and increase administrative work. Therefore, patient collections have become a major billing challenge.
Price Transparency Tasks
Price transparency requirements add another layer of complexity to billing in 2026. Providers must supply accurate cost estimates before services are delivered. In fact, creating these estimates requires detailed benefit and coverage information. As a result, patient dissatisfaction and disputes increase when estimates are inaccurate. Therefore, managing transparency responsibilities alongside routine billing tasks adds to the administrative workload and operational pressure.
Outdated Billing Systems
Many healthcare providers continue to rely on outdated billing systems in 2026. These systems often lack automation, real-time eligibility checks, and seamless updates. As a result, manual processes increase errors and slow claim submission. Also, technology limitations make it harder to meet modern payer expectations. Therefore, outdated systems remain a significant contributor to billing delays and revenue challenges.
Shrinking Reimbursement Rates
Reimbursement pressure continues to intensify in 2026 as Medicare and some commercial payers reduce or limit payment rates. Though operating costs continue to rise, reimbursement does not always keep pace. As a result, billing teams must work harder to capture every payable dollar accurately. Even minor billing errors now have a greater financial impact. Therefore, lower margins increase the importance of clean claims, faster collections, and reduced rework across billing operations.
Data Interoperability and Information Exchange
Data interoperability requirements create additional billing challenges in 2026. Providers must ensure accurate and timely exchange of patient and authorization data across systems. When systems fail to communicate appropriately, billing errors and claim delays increase. Inconsistent data can also affect prior authorizations and the accuracy of documentation. Therefore, managing interoperability adds operational complexity and requires stronger coordination between clinical, technical, and billing teams to maintain billing efficiency.
One Stop Solution for U.S. Healthcare Providers
Offshore medical billing and coding services in India offer a one-stop solution for U.S. healthcare providers facing growing complexity in 2026. These service providers provide access to trained billing and coding specialists who stay up to date with CPT, ICD-10, and payer-specific requirements. This allows healthcare organizations to maintain billing accuracy without the burden of hiring, training, or retaining in-house staff. As a result, providers can reduce errors, limit claim denials, and stabilize revenue cycles.
Additionally, partnering with experienced outsourcing medical billing and coding service providers in India, such as InfoHub Consultancy Services, helps providers manage compliance, denial prevention, and documentation accuracy more effectively. ICS delivers structured workflows, quality checks, and scalable support tailored to U.S. billing standards. This enables faster claim processing, improved collections, and better cost control. Therefore, healthcare providers can maintain financial efficiency amid increasingly challenging billing scenarios by outsourcing medical billing and coding services.
FAQs
Is in-house billing still practical for all providers in 2026?
Rising costs and complexity make in-house billing harder to manage efficiently.
Why do providers need billing expertise beyond basic coding knowledge?
Modern billing requires understanding payer rules, compliance, and reimbursement structures.
Can outdated billing workflows still work in 2026?
Manual workflows struggle to meet modern payer expectations and approval timelines.
Why is billing accuracy more important than billing speed in 2026?
Incorrect fast claims are denied more often, while accurate claims protect revenue.
Why are providers re-evaluating their billing strategies in 2026?
The reason is that the traditional billing approaches no longer align with modern payer demands.

 Medical Billing
Medical Billing  7 mins read
7 mins read