Medical Billing Services for USA Healthcare Providers (Offshore India Team)
Medical billing is where clinical work becomes collected revenue. If a claim is delayed, denied, or underpaid, the impact shows up quickly in cash flow, staffing pressure, and patient billing issues.
InfoHub Consultancy Services is an India-based offshore medical billing company supporting USA healthcare providers including hospitals, clinics, physicians, doctors, practitioners, and specialty practices. We help organizations outsource medical billing to India so they can reduce denials, improve collections, and strengthen the full RCM cycle in medical billing without building a larger in-house billing department.
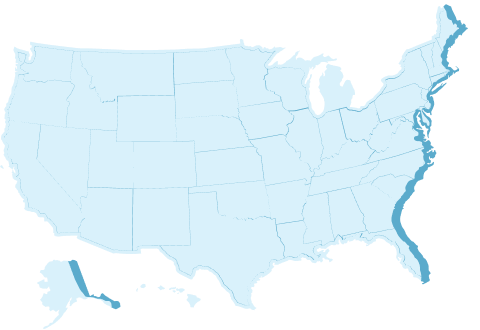
We support providers across the United States, including high-volume markets such as California, Texas, Florida, New York, Illinois, Georgia, Arizona, Washington, New Jersey, and Pennsylvania, while operating from India (Coimbatore and Chennai).

 Medical Billing
Medical Billing 


















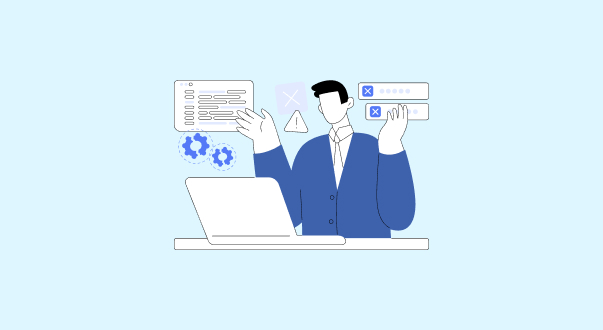



 Trusted by 140+ Providers in All 50 States
Trusted by 140+ Providers in All 50 States