RCM Healthcare (Revenue Cycle Management in Healthcare)
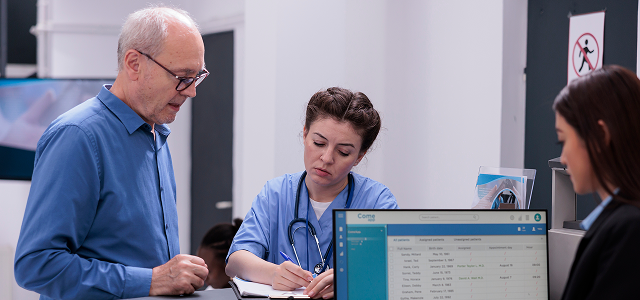
RCM healthcare is the full financial workflow that turns patient care into accurate reimbursement. If you’ve ever asked “what is RCM in healthcare?” or “what is revenue cycle in healthcare?”, the simplest answer is this:
Revenue cycle management in healthcare is everything that happens from the moment a patient schedules an appointment to the moment the final payment is collected and posted.
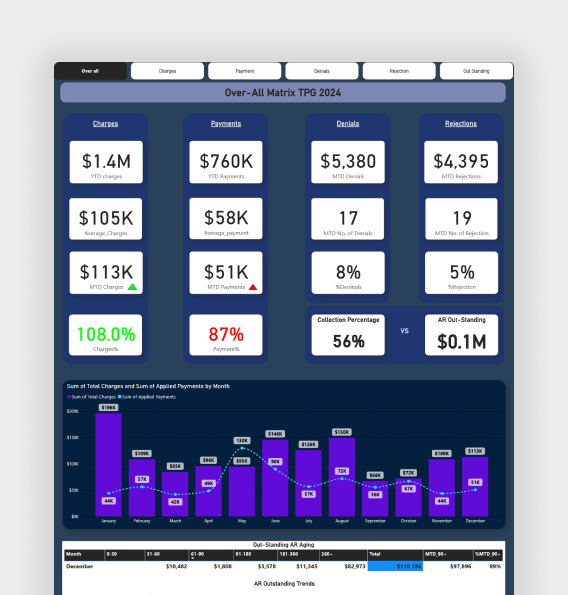
For many practices and facilities, the biggest revenue leaks come from small breakdowns: eligibility errors, missed authorizations, coding mismatches, claim rejections, underpayments, and slow A/R follow-up. That’s why many providers now use healthcare revenue cycle outsourcing to stabilize collections and reduce administrative load.
Info Hub Consultancy Services (ICS) is an offshore medical billing and healthcare RCM company supporting outsourcing from the USA to India. We help healthcare providers improve cash flow, reduce denials, and build a cleaner, more predictable billing operation without growing internal headcount.

 Medical Billing
Medical Billing 







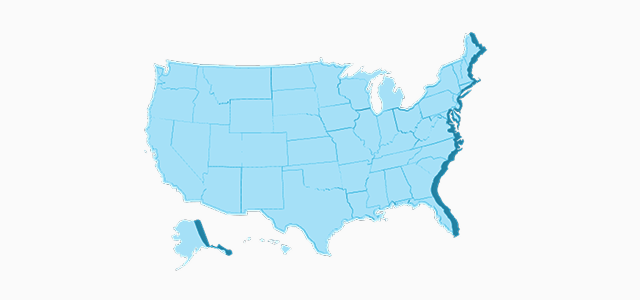


























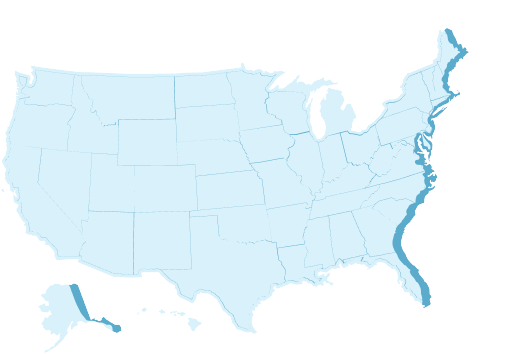
 Trusted by 140+ Providers in All 50 States
Trusted by 140+ Providers in All 50 States