Specialty medical practices operate in a high-pressure environment where every claim, code and compliance detail directly impacts revenue. As healthcare services become more specialized, billing has moved far beyond basic claim submission.
In fact, each specialty now faces its own coding rules, documentation standards, and payer expectations, making billing accuracy a constant challenge rather than a one-time task. When these complexities are not managed correctly, practices experience delayed reimbursements, rising denial rates and increased administrative workload. At the same time, providers are expected to deliver quality care while navigating tighter margins and stricter regulations. This has shifted the focus from simply managing billing to optimizing it.
Offshore billing and coding partners like InfoHub Consultancy Services help bridge this gap by delivering specialty-specific expertise, structured workflows, and consistent oversight. With the right billing support in place, healthcare practices can protect revenue, reduce operational stress, and create a more sustainable financial future.
How InfoHub Supports Specialty-Specific Billing Needs
InfoHub Consultancy Services provides tailored billing solutions to meet the unique requirements of different medical specialties. In fact, ICS ensures accurate coding, faster reimbursements, and reduced administrative burden for healthcare providers. This approach helps practices maximize revenue while maintaining compliance.
-
Specialty-Focused Expertise
ICS assigns dedicated teams trained in specific medical specialties. Consequently, each team understands the unique coding systems, payer rules, and procedural requirements of their assigned specialty. This focused knowledge allows healthcare providers to rely on precise billing practices that minimize errors and support accurate reimbursement for complex medical services.
-
Accurate Coding & Documentation Review
Accurate coding is critical for specialty billing, and ICS ensures thorough review of patient records and documentation. ICS assigns the correct CPT, ICD-10, or HCPCS codes by carefully verifying clinical notes and service details. This process reduces claim denials, accelerates payments, and maintains compliance with payer regulations.
-
Customized Billing Workflows
Each specialty has unique billing needs, and ICS creates workflows tailored to these requirements. Their processes streamline claim preparation and submission by integrating with practice management systems and electronic health records. This customization enhances efficiency, minimizes errors, and allows healthcare staff to focus more on patient care rather than administrative tasks.
-
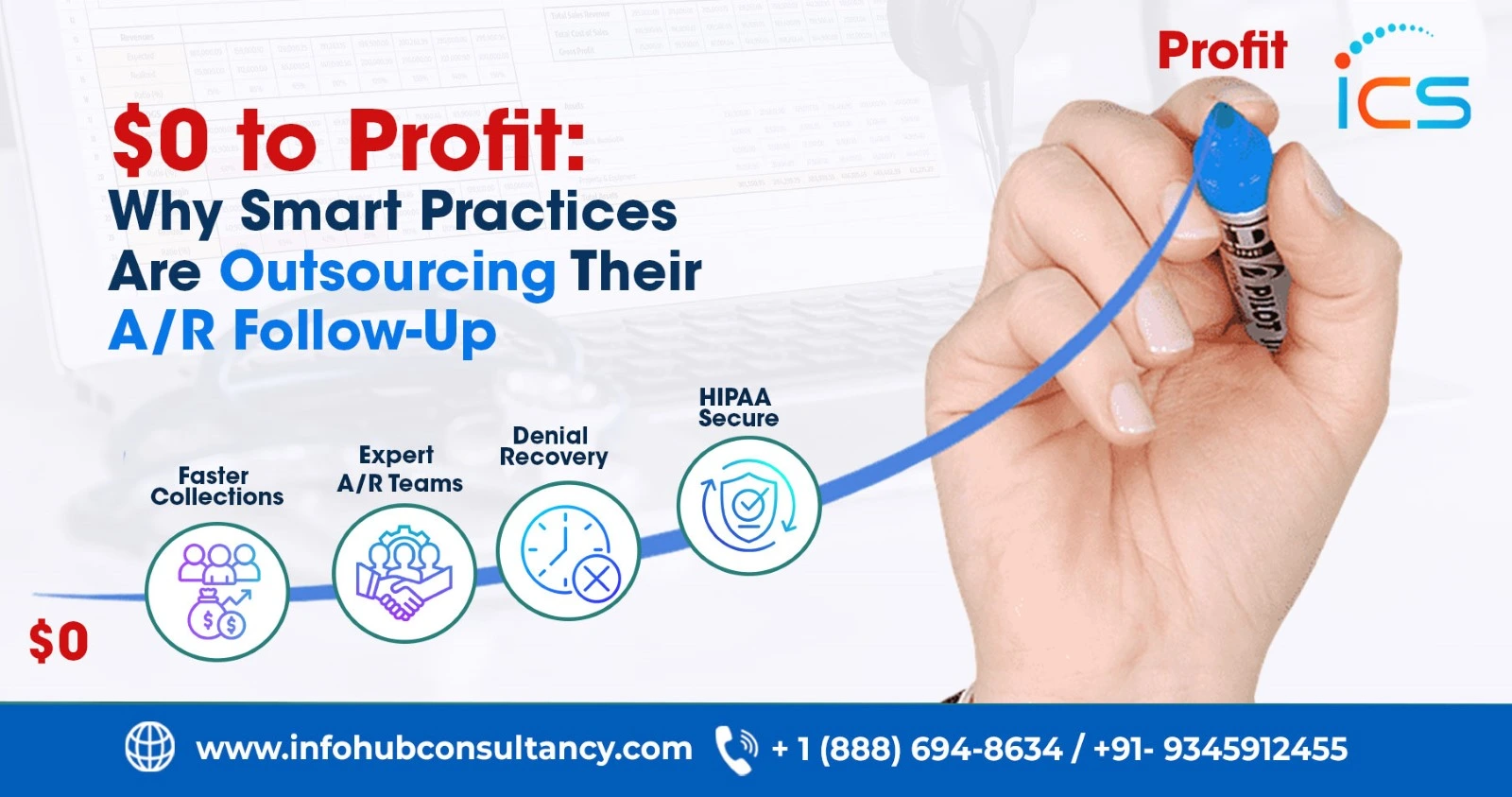
Denial Management & Claims Follow-Up
ICS proactively monitors submitted claims to detect denials or rejections. Their team investigates the causes, corrects errors, and resubmits claims promptly. Moreover, ICS helps practices recover revenue faster, reduces administrative strain, and ensures specialty-specific claims meet payer requirements without repeated delays by efficiently handling follow-ups.
-
Reporting & Analytics
ICS provides specialty-focused reports and dashboards that highlight key performance metrics, including collections, denials, and reimbursement trends. Through detailed analytics, practices can identify patterns, improve billing efficiency, and make informed decisions. These insights support better revenue management while ensuring compliance with healthcare regulations.
-
Compliance & Regulatory Support
Navigating complex regulations is essential in specialty billing. ICS ensures adherence to HIPAA, CMS, and payer-specific guidelines for each specialty. In fact, they minimize compliance risks, reduce audit exposure, and help practices avoid penalties by continuously updating their processes while maintaining accurate and secure financial records.
-
Cost-Effectiveness & Scalability
Utilizing offshore resources, ICS provides cost-efficient billing solutions that reduce operational expenses. Additionally, their teams scale easily to accommodate growth or fluctuating workloads. This flexibility allows healthcare providers to maintain high-quality billing services without hiring additional staff, ensuring efficient management of specialty-specific billing needs.
How Specialty Billing Works: Process Steps?
Specialty billing involves multiple steps that ensure accurate, compliant, and timely reimbursement. ICS follows a systematic process that combines clinical expertise and technology. In fact, each stage is designed to handle the specific requirements of a specialty, reduce errors, and optimize revenue. Thereby, clear procedures support smoother operations and better financial outcomes.
-
Patient Data & Documentation Intake
ICS begins by collecting all relevant patient information and clinical documentation. This includes visit notes, lab reports, and procedure details. Also, they lay the foundation for precise coding by accurately organizing records. As a result, proper intake ensures that every claim submitted is complete, reducing rejections and facilitating faster reimbursement.
-
Specialty-Specific Code Assignment
Using dedicated expertise, ICS assigns the correct CPT, ICD-10, or HCPCS codes for each service. This step considers the specialty’s unique procedures, modifiers, and payer rules. Accurate coding ensures claims are accepted on the first submission, improves reimbursement rates, and reflects the complexity of care provided by the practice.
-
Quality Review & Compliance Check
Before submission, each claim undergoes a thorough quality review to verify accuracy and adherence to regulatory standards. ICS checks documentation, coding, and payer guidelines to prevent errors. This ensures compliance with healthcare regulations, reduces audit risk, and supports smooth specialty-specific billing claim processing.
-
Claims Submission & Tracking
Once verified, claims are submitted electronically to the appropriate payers. InfoHub Consultancy Services tracks each claim throughout the reimbursement cycle, monitoring approvals and payments. In fact, continuous tracking ensures that any delays or issues are addressed immediately, maintaining cash flow and supporting financial stability for specialty practices.
-
Denial Analysis & Resolution
When a claim is denied, ICS analyzes the reason and takes corrective action. They update documentation, adjust coding if necessary, and resubmit promptly. Thereby, ICS helps practices recover revenue, reduce administrative workload, and maintain compliance with specialty-specific payer requirements by addressing denials efficiently.
-
Reporting & Continuous Improvement
Finally, ICS generates reports on collections, denials, and key billing metrics. These analytics provide insights into trends, areas for improvement, and specialty-specific challenges. Practices can use this information to enhance workflows, increase reimbursement efficiency, and ensure long-term financial performance.
Role of InfoHub Consultancy Services
InfoHub Consultancy Services acts as an outsourcing medical billing and coding service provider in India for healthcare practices by addressing the financial and operational challenges of specialty-specific billing. Instead of simply processing claims, ICS aligns its services with each practice’s goals, ensuring accurate revenue capture, regulatory compliance, and efficient workflow management. Their guidance helps providers focus on patient care while optimizing financial performance.
Moreover, the company brings deep industry knowledge and specialty-specific insights to every engagement. Also, ICS helps practices adapt to changing payer requirements, streamline reimbursement strategies, and reduce administrative complexity by understanding the complexities of various medical fields. This consultative role ensures that practices not only receive accurate billing support but also improve overall operational efficiency and long-term sustainability.
Additionally, ICS enhances transparency and decision-making through detailed analytics and reporting. Practices gain actionable insights into revenue trends, claim performance, and compliance gaps. Therefore, ICS transforms specialty billing from a routine administrative task into a value-driven process that strengthens financial stability and supports practice growth.
FAQs
What makes specialty-specific billing different from general medical billing?
Specialty billing requires deeper knowledge of procedure complexity, modifiers, and payer-specific reimbursement rules.
Can InfoHub Consultancy Services support multi-specialty practices under one billing model?
ICS offers coordinated billing support while maintaining specialty-level accuracy for each service line.
How does offshore billing improve turnaround time for specialty claims?
Round-the-clock offshore operations enable faster claim processing and follow-ups without workflow interruptions.

 Medical Billing
Medical Billing  6 mins read
6 mins read