Durable Medical Equipment Billing or DME billing plays an important role in the U.S. healthcare reimbursement process. It is a detailed process that directly impacts the financial health of DME providers and the continuity of patient care.
Did you know? As per CMS, DME providers encounter a 35% denial rate of DME claims on the very first submission. Such denial is due to inaccurate coding, incorrect documentation, or failure to fulfill the medical necessity requirements. In fact, these errors not only lead to delayed healthcare reimbursements but also to compliance audits.
Accurate DME billing is now critical than ever, given the rising scrutiny from payers, the increase in audit activities, and the growing demand for accountability in DME services. As billing guidelines continue to evolve and compliance expectations tighten, DME providers need to understand the most common errors and how to avoid them.
In this blog, we will outline the best practices that can be used to minimize frequent DME billing claim errors and maximize claim acceptance rates.
Understanding Best Practices in DME Billing
DME providers must adopt a structured and detail-oriented billing process to reduce errors and speed up reimbursements. The following are the best practices to help in effective and compliant DME billing.
- Accurate Coding and Documentation
One of the most frequent reasons for claim denials is incorrect or incomplete coding. Use of outdated HCPCS or CPT codes, missing modifiers (like KX, GA, or RT/LT), or failing to assign codes to valid documentation can all lead to financial issues. Thereby, it is crucial to ensure that each billed item supports a valid prescription or clear clinical notes. In fact, these documents are evidence of the medical necessity and duration of use for the equipment. Keeping coding and documentation aligned helps DME providers to reduce common errors, ensures faster payments, and protects your practice from financial setbacks due to non-compliance.
- Proper Maintenance of Patient Records
Maintaining thorough and well-organized records of the patients is important, especially during audits and appeals. Each patient file should comprise all necessary medical-related documents, such as written orders, progress notes, delivery receipts, and authorizations. In fact, the billing team needs to ensure that each document is properly signed and dated in sequence. Using a digital documentation system can be the best solution to store, retrieve, and review the records more easily. All this will improve data security and ensure compliance with payer and regulatory requirements.
- Monitoring and Follow-Up on Claims
After submitting DME claims, the billing and coding team must follow them from time to time to check their status. Any denials, delays, or underpayments should automatically prompt a review to determine the reason and resubmit it correctly. Also, timely intervention prevents delayed payment cycles and lost revenue. Additionally, setting up a system for ongoing A/R (Accounts Receivable) follow-up, appeal, and secondary billing assists in resolving the pending claims appropriately. This ensures cash flow and avoids revenue loss.
- Compliance with Coding Guidelines
Adhering to payer-specific billing and coding guidelines is critical to remain compliant and prevent claim denials or audits. The DME billing and coding staff should check coding updates and policy changes periodically to prevent billing of non-covered items or services. Providers also sometimes unknowingly submit improper claims as they don’t know about the updated changes. Therefore, constant staff training and quarterly coding audits are necessary. This guarantees proper DME billing with high reimbursements and low audit risks.
- Timely Submission of Claims
Late submissions of DME claims can automatically result in claim denials or reduced payments. Each payer has a specific filing window, so submitting claims within those timelines is essential. Claims filed even a few days late can be denied. To prevent this, billing teams should adopt automated reminders or scheduling tools to alert them before critical due dates. Also, submitting claims in smaller, more frequent batches rather than waiting to submit in bulk can improve turnaround time and help identify issues early.
- Verification of Insurance Coverage
It is best to thoroughly verify the patient’s insurance information before providing any equipment or service. This includes verifying whether their insurance is active, how much they have to pay as their deductible, if prior authorization is required, and how much they will pay out of pocket. This prevents denials of the claims and informs the patient how much they should pay. Using technology such as real-time eligibility checking or systems that connect directly with insurance databases can speed up the process and make it more accurate. It not only saves time but also allows the provider and patient to be on the same page from the beginning.
Conclusion
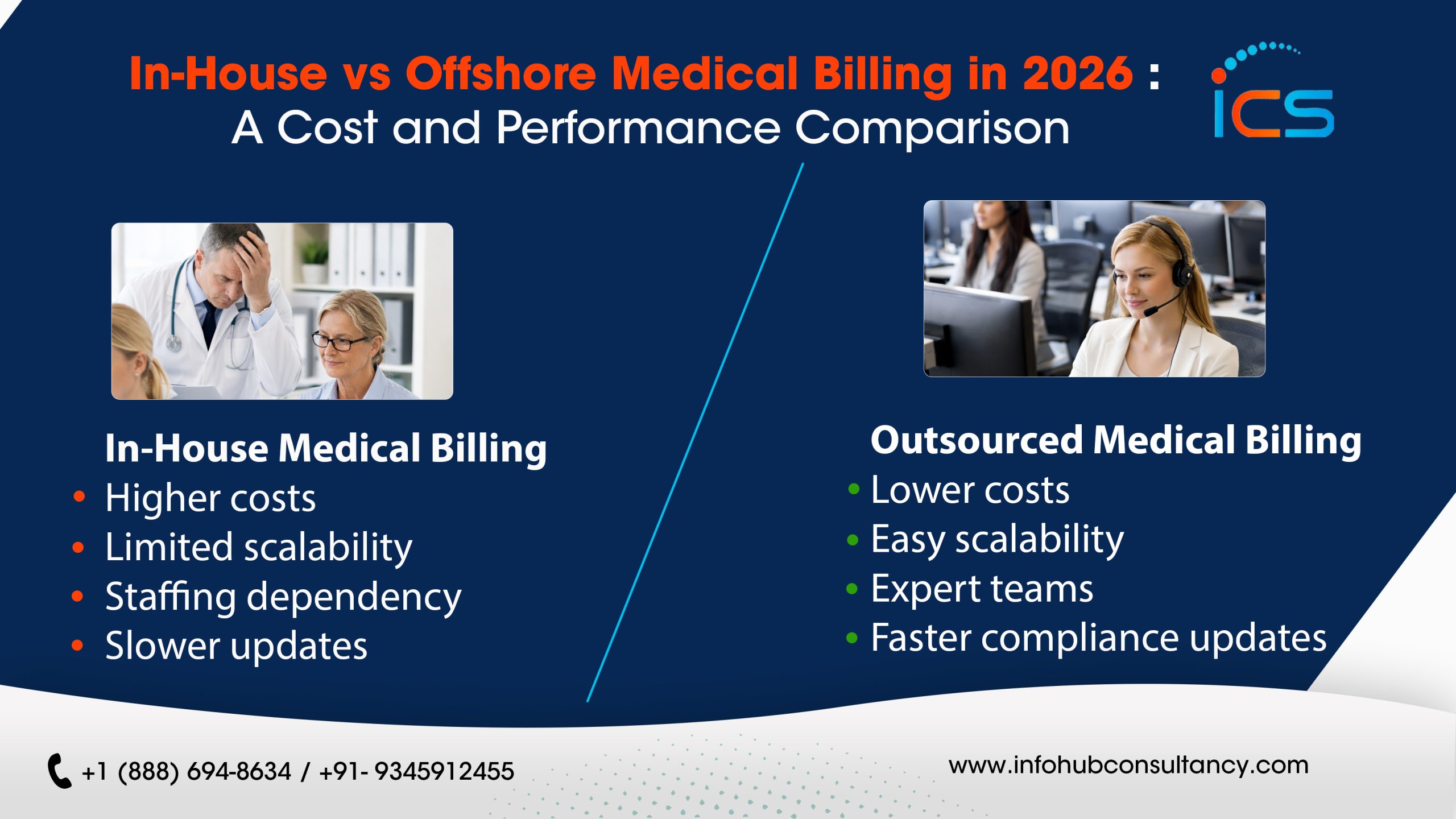
Outsourcing medical billing and coding services providers in India can significantly improve the accuracy of the claim submission and healthcare reimbursement for the DME providers. Instead of juggling claim submissions, coding rules, and follow-ups, you can hand the work to professionals who undertake daily DME billing and coding tasks.
However, before outsourcing DME coding and billing, you should ask:
Does your outsourced offshore partner conduct real-time eligibility checking? Can the billers and coders customize billing solutions based on your practice type and specialty? Are they able to recognize errors or issues before submission?
If yes, outsourcing offshore medical billing and coding services in India is the most viable solution. One such offshore partner is InfoHub Consultancy Services, which has highly trained DME billers and coders who know which DME codes to apply, how to process denials, and when the forms are incomplete. Our team also remains updated on all Medicare guidelines and insurance company updates, so there is a high chance of getting the claims approved the very first time.
FAQs
1. What are the most frequent DME billing errors?
Some of the most frequent errors are Improper documentation, inaccurate codes, not including modifiers, and delay in billing.
2. How do I ensure proper documentation for DME billing?
Do ensure that you have signed orders, medical necessity documentation, delivery reports, and all relevant CMNs. Also, double-check documents and dates against each claim’s information.
3. What is the purpose of modifiers in DME billing?
Modifiers like GA, KX, and RT/LT provide additional information that determines claim acceptance, as incomplete or faulty modifiers are the causes for denials.
4. Why is insurance verification necessary before submitting claims?
It confirms coverage, co-pays or deductibles, and pre-authorization needs, preventing future claim issues.
5. Can outsourcing DME billing reduce audit risks?
Yes. Outsourced partners such as ICS stay up to date on payer rules, code changes, and compliance guidelines, reducing mistakes and enhancing submission accuracy.

 Medical Billing
Medical Billing  6 mins read
6 mins read