Managing revenue has become increasingly challenging for small medical practices, especially as claim denials continue to rise each year. In 2023, around 19% of in-network claims submitted under insurance plans were denied on the first attempt. In the broader healthcare system, many providers experience initial denial rates of 10% to 15%, which can be even higher depending on the payer. These denials are more than just administrative setbacks, as ongoing errors can lead to a 5–15% annual revenue loss.
Such revenue risks can quickly disrupt cash flow and overall stability for small practices operating with limited financial and staffing resources. As a result, adopting a cost-effective RCM approach becomes essential rather than optional. This blog explains how small practices can implement practical and affordable RCM solutions that deliver measurable improvements without stretching their budget.
RCM Solutions for Small Practices on a Smaller Budget
Small practices often struggle to balance efficient RCM with limited financial and staffing resources. However, they can significantly improve billing accuracy, reduce denials, and strengthen overall cash flow by adopting practical, low-cost strategies.
1.Enhancing Front-End Processes
Improving front-end operations is one of the most affordable ways for small practices to increase revenue as most claim problems start at this early stage. When administrative tasks are handled correctly from the beginning, practices experience a smoother billing flow that supports faster reimbursement and better cash management.
- Streamlined Patient Registration
A well-organized registration process ensures that staff collect accurate demographic and insurance details right at the start. When this information is complete, the billing team spends less time correcting errors later. As a result, claims move through the system smoothly, and the practice avoids unnecessary payment delays and preventable denials.
- Real-Time Insurance Verification
Real-time insurance checks allow staff to confirm eligibility, deductibles, and coverage rules before the patient is seen. This step prevents issues related to outdated or incorrect insurance information. As a result, practices face fewer eligibility-related denials, and patients gain a clearer understanding of their financial responsibility, helping keep payments on track.
- Accurate Benefits Capture
Capturing benefits early helps practices understand how much the patient’s plan will cover and what the patient must pay out of pocket. When this information is shared upfront, patients feel more informed and prepared to pay their portion on time. Therefore, practices experience fewer disputes, fewer delays, and more predictable financial outcomes.
- Using Front-Desk Staff Checklists
Front-desk checklists guide staff through each step of the intake process to ensure that nothing is overlooked. This simple tool helps maintain consistency and reduces the chances of missing critical details. As a result claims are submitted more accurately, strengthening first-pass approval rates and improving overall revenue generation.
2.Improving Medical Coding Accuracy
Accurate coding is essential for clean claim submission, and small practices can achieve strong results even without hiring experienced coders. Consequently, practices can maintain compliance and minimize denials while still working within a limited budget.
- Utilizing Free or Affordable Coding Resources
Small practices can take advantage of free CMS updates, affordable coding tools, and EMR-integrated code suggestions to stay compliant with billing rules. These resources help staff understand changing guidelines without the expense of training. As a result, coding accuracy improves, and the practice avoids denials caused by outdated or incorrect coding information.
- Standardized Coding Templates
Standardized templates make coding easier by creating a consistent format for commonly performed procedures. In fact, they reduce the chance of variation or incomplete coding when staff follow these templates. Therefore, claims are more uniform, easier to audit, and more likely to be accepted on the first submission, improving efficiency and reimbursement speed.
- Routine Staff Education
Free webinars, payer newsletters and professional bulletins provide staff with continuous learning opportunities without increasing costs. These updates help them understand new rules, code changes and common billing pitfalls. Consequently the practice stays aligned with industry standards and reduces the risk of denials related to outdated knowledge or incorrect coding choices.
- AI-Assisted Coding Features
Many affordable RCM systems now include AI tools that highlight potential coding or documentation issues before claims are submitted. These alerts act as an additional layer of protection, especially for small teams with limited coding expertise. As a result, errors are caught early, and the practice can maintain strong accuracy without hiring additional specialists.
3.Strengthening Charge Capture and Documentation Practices
Effective charge capture ensures that every service provided is billed correctly, which is essential for maintaining stable revenue. Also, practices avoid missed charges and coding errors when documentation is complete and accurate.
- Using EMR Templates and Macros
EMR templates and macros guide providers to document all relevant details for each visit. This helps them capture the full complexity of the patient encounter and ensures charges reflect the services performed. As a result, undercoding decreases, documentation improves and claims accurately represent the level of care delivered.
- Daily Charge Reconciliation
Daily reconciliation compares provider schedules with the charges submitted to ensure no services are missed. This routine prevents overlooked visits or procedures from going unbilled. Over time this consistent review helps practices maintain complete revenue capture, reduce financial waste and improve overall billing accuracy.
- Provider Documentation Education
Training providers on proper documentation helps them understand which details support accurate coding and billing. When providers document clearly and thoroughly, it strengthens the coding process and reduces billing disputes. Therefore, this leads to better claim approval rates, improved compliance, and more accurate reimbursement.
- Implementing Checklists
Checklists for common visit types help providers and staff follow a predictable documentation pattern. These tools ensure that essential elements are consistently included in each encounter. As a result practices avoid missing details that could delay claims or weaken the accuracy of submitted codes.
4.Using Affordable RCM Technology
Budget-friendly RCM tools give small practices access to features that streamline billing and minimize costly errors. Even low-cost systems now offer robust functionality that improves claim submission, payment processing, and communication.
- Cost-Effective Cloud-Based Systems
Cloud-based solutions offer subscription pricing, reducing upfront costs and eliminating the need for hardware installations. These systems often include automatic updates and built-in security features. As a result small practices gain access to powerful billing functions while keeping long-term expenses predictable and manageable.
- Electronic Claims and Auto-Scrubbing
Electronic claim submission and auto-scrubbing tools identify common errors before claims reach the payer. This early detection helps prevent rejections and reduces the time spent on rework. When claims are cleaner from the beginning, practices benefit from faster payments and fewer administrative burdens.
- Digital Payment Portals
Digital payment portals offer patients a convenient way to make payments anytime, which significantly increases collection speed. These portals also reduce the manual work required to process checks or handle in-person payments. As a result, the practice improves its cash flow while enhancing patient satisfaction.
- Built-In RCM Features
Affordable billing software often includes automatic eligibility checks, coding alerts and error notifications. These built-in tools help staff avoid mistakes and submit cleaner claims. Consequently, even small teams can maintain a smooth billing process without relying heavily on manual review or extensive training.
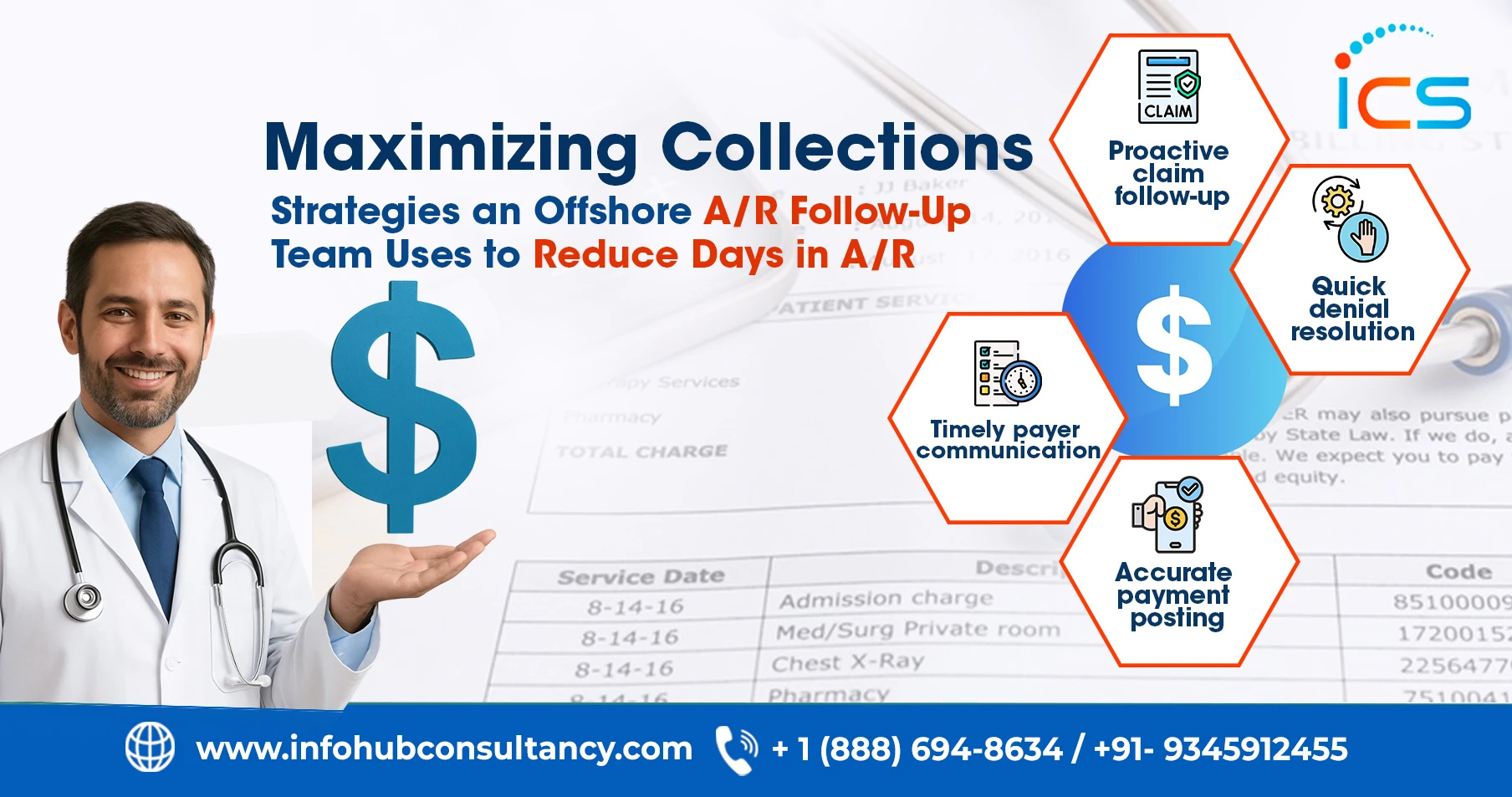
Leverage Offshore Medical Billing and Coding Services in India
Outsourcing medical billing and coding services allows small practices to improve efficiency without hiring or training additional staff. This approach is budget-friendly as practices only pay for the exact level of support they need while gaining access to experienced billing professionals. Moreover outsourcing reduces common errors, lowers denial rates and speeds up collections. Small clinics can partner with reliable outsourcing medical billing and coding service providers in India such as InfoHub Consultancy Services, which offer affordable and high-quality RCM support that strengthens overall financial performance.
FAQs
How can small clinics reduce billing turnaround time affordably?
By simplifying internal handoffs and ensuring tasks move quickly from one step to the next.
Does patient education support low-cost RCM improvement?
Informed patients are more likely to follow payment timelines and provide accurate details.
Can small practices follow a simple monthly RCM checklist?
A short checklist keeps the revenue cycle organized and prevents missed steps.

 Medical Billing
Medical Billing  7 mins read
7 mins read